How Our Vision For a Digital Health Strategy Will Transform the Military Health System
This article is the first in a four-part series that explores leading practices for the MHS around developing and implementing a digital health strategy along the care continuum.
 |
| Graphic credit: Sofia Echelmeyer, USU |
August 29, 2023 by Dr. Lester Martínez-López, Lt. Gen. (Dr.) Telita Crosland and Dr. Jonathan Woodson
Much like the broader health care system in the United States, the Military Health System (MHS) is facing projected increases in costly chronic conditions such as diabetes among the millions of beneficiaries it serves, along with a looming shortage of clinicians and caregivers. For the MHS, these and other challenges not only present cost and care delivery pressures; they also have a significant impact on military readiness and the readiness of the medical force — both vital to deterring our adversaries and protecting our interests and allies around the world.
Organizations across today’s health care landscape are increasingly engaging in digital transformation to improve patient experience and outcomes, minimize clinician burnout, reduce costs, advance health equity, and tackle other longstanding clinical and operational challenges. Companies across a wide spectrum -- from long-established health systems to new market entrants -- are disrupting health care by digitalizing key processes such as scheduling appointments, ordering tests or medications, and facilitating communications between patients and providers.
Given these successes, the MHS has a significant opportunity to reimagine care delivery by weaving digital into every aspect of the organization (rather than executing unrelated technology projects) and envisioning the future of the MHS as a portfolio of multiple solutions in a single ecosystem (i.e., a network of digital tools, service providers and products that work together to create value). In addition to improving patient outcomes, military readiness and morale among our service members, digital transformation can help advance the National Defense Strategy’s stated goal of maintaining American dominance across technology and innovation in crucial domains.
The MHS will need to take a strategic approach to redesigning its current care models to enable this vision and enable more safe, effective, efficient, equitable and patient-centered care.
Developing a long-term digital vision for the MHS
To build such a digital ecosystem, the MHS will need to first consider all the skillsets and capabilities necessary along the medical and health lifecycle of active-duty personnel and other beneficiaries. This vision must be guided by a common set of rules and principles addressing governance, user centricity, security, and interoperability and common nomenclature and standards across data platforms. It also needs to allow for the flexible integration of new tools and applications into the ecosystem, including those from third parties.
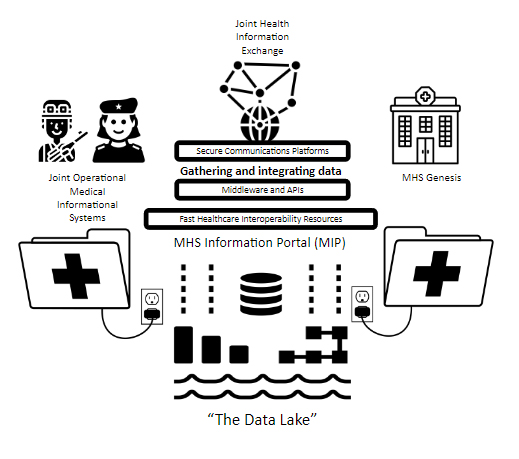
A key component of any robust digital ecosystem, the enterprise resource planning system is a digital platform that acts as the “glue” that holds an ecosystem together, creating value by enabling the exchange of information, services or currency among patients, clinicians, administrators, back-office functions and other stakeholders. While today’s MHS utilizes several different platforms that are not interconnected or interoperable in this way, the MHS digital health ecosystem of the future can be linked across solutions, addressing the active-duty service continuum across soldier fitness, readiness and preventive care in a diverse array of locations, including beneficiaries’ own homes, military treatment facilities and deployed settings.
For example, the Joint Operational Medical Information System (JOMIS), the expeditionary version of the MHS’ new electronic health record (referred to as MHS Genesis) includes a suite of platforms designed to meet the unique challenges of documenting and coordinating health care in the deployed environment. As a future use case, the periodic health assessments required for active-duty personnel and reservists could be administered digitally and reduce lost time at duty stations, the need for in-person visits, and the need for provider time and associated costs.
As these and other technology enhancements are developed and deployed, MHS leaders need to reconcile their long-term vision of a digitalized MHS with the current state of the MHS environment and system, formulating a plan to close gaps and benchmark progress. Moreover, their vision needs to be flexible enough to incorporate innovative technologies and service delivery trends (e.g., generative artificial intelligence, augmented and virtual reality, virtual care, telehealth experiences) that are still emerging and need to be evaluated.
Activating our digital strategy
Given the complexity and size of the MHS, an incremental approach to digital transformation will allow for future technologies to be introduced as the ecosystem evolves. Because standing up major change programs can take several years, taking a flexible and agile approach that enables the MHS to evolve as technology matures and our understanding grows around the value of a digital health ecosystem will be key.
In accordance with the US National Defense Strategy, the Department of Defense continuously invests in, plans for and implements prominent high-tech programs to maintain technological dominance. For example, the DoD’s Joint Artificial Intelligence Center (JAIC) is charged with accelerating and implementing artificial intelligence initiatives at scale for the MHS’ procurement and implementation of MHS Genesis. These efforts will provide lessons learned and other key insights around the planning and implementation of the MHS digital ecosystem.
Below are three key actions to begin activating our digital health strategy, gleaned from this JAIC work and other initiatives:
- From the outset, formulate an overarching strategic vision for the military health system’s digital health ecosystem and establish key success criteria for its planning and implementation akin to those recommended by the Government Accountability Office high-tech Department of Defense initiatives.
- Establish a roadmap that incorporates all relevant projects into the overall strategy, outlining roles and responsibilities for effective collaboration, identifying the tech and operational platforms to be used or tested, and providing other guidelines via a phased approach.
- Focus and concentrate the necessary resources, both financial and technical, to create a fully digitally integrated and maximally effective military health care system.
 |
| (Graphic courtesy of the Defense Health Agency) |
Summary
As the “way of war” continues to evolve, so must the MHS and its approach to caring for the men and women who put themselves in harm’s way to protect the ideals our country holds so dear. By reimagining military health within a single digital ecosystem that improves care delivery and outcomes for our people around the world, we will not only create value and boost military readiness; we will also honor our service men and women for their incredible sacrifice.


