Revolutionizing Shoulder Instability Research with 3D MRI Imaging and AI
Advanced MRI imaging and AI learning models are transforming the study of shoulder instability, potentially improving treatment for a debilitating cause of injury in military personnel.
June 24, 2025 by Hadiyah Brendel
Shoulder instability—when the shoulder joint slips out of place or dislocates—is a common and serious injury among service members, affecting their ability to stay mission-ready. It's one of the top musculoskeletal injuries in the military. The Uniformed Services University’s (USU) Musculoskeletal Injury Rehabilitation Research for Operational Readiness (MIRROR) program is working to improve care and prevention through research, education, and training centered around several of these types of common joint and muscle injuries.
MIRROR Project 6, titled “Early Identification of Glenohumeral Pathomorphology to Prevent Recurrent Shoulder Instability,” one of 84 current MIRROR research projects, studies shoulder instability to inform optimal treatment measures through integration of high-resolution 3D models from MRI data and AI machine learning tools.
This project focuses on detecting structural abnormalities and potential indicators of instability, to help prevent repeated shoulder dislocations in service members. Specifically, it looks at the main shoulder joint–the glenohumeral joint—where the top of the upper arm bone (the humerus) fits into a shallow socket of the shoulder blade, known as the glenoid. Identifying issues in this area early on can help reduce the risk of ongoing shoulder problems.
“Think of the shoulder joint like a golf ball and tee,” says Matthew Bradley, Program Manager for the MIRROR Project 6 study. “The ball is cupped by the tee, providing some stability, and together this ball-and-socket structure allows for a wide range of shoulder motion. But, if part of the tee chips off, the ball can fall off more easily.” Bradley further explains, “Whenever the shoulder pops out, there’s injury to the soft tissue structures, and some bone of the glenoid may chip off as well, making it easier for future instability events to occur.
Losses of bone and other structural integrity leads to a high rate of re-injury. When compared to the civilian population, military trainees have significantly higher risk, being 20 times more likely to experience an instability event. Further, around 80% of these individuals commonly experience re-injury to the shoulder. Recurrent instability heightens risks, leading to more bone loss, surgical failures, and post-traumatic arthritis.
The research involves examining the structural changes within the glenohumeral joint that may result from shoulder instability events. Additionally, the study team is working to identify and understand naturally occurring morphological variances that may predispose an individual to injury. MIRROR’s research seeks to develop military-specific clinical practice guidelines (CPGs) to optimize treatment, improve patient outcomes, and maximize return to duty for service members.
MIRROR Project 6 is a longitudinal study, aiming to examine early-career service members over the course of their entire military career. This study recruited and enrolled participants within their first year of entering the following service academies: the U.S. Air Force Academy (USAFA), the U.S. Military Academy (USMA), or the U.S. Naval Academy (USNA). This long-term approach allows researchers to track shoulder health and injury development over time, hoping to gain understanding into the long-term effects of shoulder instability on service members’ careers.
Traditional methods of diagnosis and treatment have limitations. CT scans are commonly used for 3D visualization and bone loss assessment. However, they involve radiation exposure, additional time, and higher costs. Alternatively, MRIs excel in generating a 2D soft-tissue assessment, but are generally less effective than a CT scan for detecting bone loss. MIRROR Project 6 is utilizing an innovative type of MRI scan that allows for both 2D soft-tissue assessment as well as 3D visualization for bone loss. Since August 2020, almost 3,000 participants have been enrolled in the study and researchers have captured over 900 bilateral shoulder MRI scans (over 1,800 scans total) using the new MRI sequence technique.
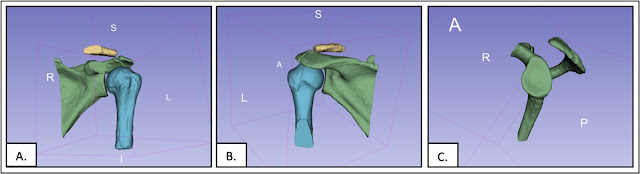
The 3D model reconstruction technique developed with the MIRROR Project 6 study utilizes 3DSlicer, a software for medical image viewing and analysis, to segment the scapula and humerus from MRI datasets, creating realistic 3D models of the shoulder joint. The 3D model allows for more in-depth analysis to assess bone loss and can help determine between surgical and non-surgical pathways, all while avoiding radiation exposure associated with CT scans. The process for manual development of a high-quality 3D model, however, currently takes approximately three hours to complete and has been led by Jacob Dowe, a Research Coordinator at USNA. This intricate work is further supported by a dedicated research team, including Audrey Hartin and Dr. Judd Robins both at USAFA, and Dr. Ken Cameron at USMA.
To assist with the 3D model creation process at scale, the MIRROR Project 6 team is collaborating with COL (Ret) Jonathan Dickens, MD, who was the former principal investigator of this study and now a sports medicine surgeon at Duke University. MIRROR and Duke are working toward building an AI learning model that automates the creation of the 3D models from the MRI scans that have already been collected. This automation will significantly reduce the time required for model generation.
The AI will also enable large-scale comparative analyses. Bradley says they are interested in identifying morphological patterns such as whether the shape and symmetry of the glenohumeral joint affect risk of instability events. Additionally, the 3D models will aid in evaluating whether pre-existing methods for assessing bone loss—such as comparing the injured shoulder to the uninjured shoulder—remain an appropriate measure for quantifying the extent of bone loss.
Bradley expresses optimism about the project’s current juncture, stating, “We’re at a really exciting point.” He believes based on the work already completed and the discoveries made, the research has the potential to fundamentally “change the course of care” for anyone who experiences a shoulder instability event, regardless if surgery is ultimately required.
While the specific aim of differentiating surgical from non-surgical candidates based on 3D models is still in the long-term surveillance phase, Bradley highlights an immediate impact: the implementation of this advanced MRI sequence itself. This 3D sequencing allows for a clearer representation of the joint from all viewing angles, when reformatted within the imaging system. Additionally, he explains that simply incorporating this into standard MRI scans and developing 3D model reconstructions can yield significantly more information than traditional 2D sequences. This enhanced visualization could directly inform surgical decision-making, allowing surgeons to more precisely identify the extent of bone loss and select the most appropriate treatment pathway from various surgical options. Conversely, if a 3D model reveals less bone loss than initially perceived on 2D scan, it might indicate physical therapy as a more viable option and potentially avoid unnecessary surgery.
“The advancements driven by MIRROR Project 6 are anticipated to enhance force medical readiness,” said Dr. Brad Isaacson, chief of research and operations for MIRROR, associate professor with the Department of Physical Medicine and Rehabilitation at USU, and principal investigator with The Geneva Foundation. “By optimizing the management of shoulder instability, this research aims to improve patient outcomes, maximize the rate at which warfighters can return to duty, and reduce the risk of re-injury among service members.”